cPTSD And Me
This is my first email from Buttondown! This is why it looks different. You can still see my archive and read online here if you prefer.
I had to do a presentation recently for my therapy training. It was an assignment for a unit on theories of counselling and mental health. I did mine on cPTSD, as that’s what I have the most experience with.
It was only 20mins so had to be high level, but thought I’d share some things I talked about, as I’ve not really talked about cPTSD in the newsletter in detail.
This turned into a bit of a beast! I'm not a qualified psychologist, just a trainee therapist who did a fair bit of research into their condition. Here's an overview of cPTSD as I experience it.
Introduction
According to the ICD11, cPTSD is described as:
Complex post traumatic stress disorder (Complex PTSD) is a disorder that may develop following exposure to an event or series of events of an extremely threatening or horrific nature, most commonly prolonged or repetitive events from which escape is difficult or impossible […].
All diagnostic requirements for PTSD are met. In addition, Complex PTSD is characterised by severe and persistent 1) problems in affect regulation; 2) beliefs about oneself as diminished, defeated or worthless, accompanied by feelings of shame, guilt or failure related to the traumatic event; and 3) difficulties in sustaining relationships and in feeling close to others.
The first psychiatrist to propose cPTSD was Judith Lewis Herman in her book, Trauma and Recovery back in 1992.
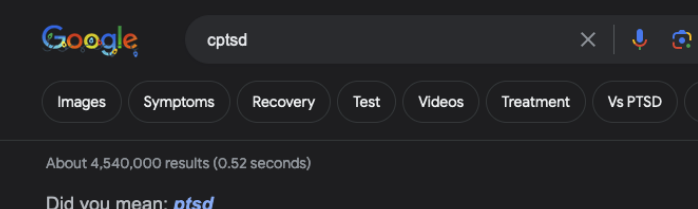
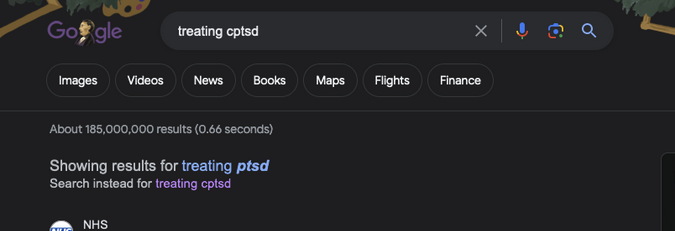
However, cPTSD has only just been included in the ICD11, and the DSM-V doesn't recognise it. The closest related condition in the DSM is the PTSD substype dissociative PTSD.
My Experience
I experience hypervigilance, dissociation, emotional flashbacks, nightmares, and persistent feelings of shame, guilt, failure and worthlessness, and difficulties in maintaining friendships and feeling secure in relationships in general.
Let’s talk about what these mean for me.
Hypervigilience (sometimes called Hyperarousal, but that sounds like a HR nightmare) is constantly assessing for potential threats. It looks like I’m distracted and fidgety, but it’s because I’m hyper aware of sounds and people around me, and I’m on edge, waiting for something to go wrong. It comes from my role as the fixer and the peacekeeper in my family. If I could fix things before people even realised there was an issue, everyone would stay happy and calm and safe. It was easier that way.
Emotional Flashbacks. You know when you have a song stuck in your head? Like that, but with the worst things you’ve ever experienced. You’re going about your day reliving terrible things, with the full emotions of that time, but you’re aware of where you are.
Hypervigilance and flashbacks meant I was avoiding certain circumstances and memories, carefully guiding my inner monologue to avoid things that would trigger a flashback, which in turn, led to dissociation.
Dissociation. This is a disconnection from thoughts, feelings, memories, or sense of indentity. For me it was a disconnection from feelings, then later memories. I didn’t have a safe space to feel my emotions at home, so I learned to push them down until I felt little at all. I’m not that bad any more, but a warning sign for me used to be when, instead of laughing at something, I’d just think ‘that’s funny’. It was an acceptance that something funny was happening, and I should be laughing, but I didn’t laugh, because I had disconnected myself.
Research
The lack of consensus on the condition and diagnosis means that there's not a huge amount of research done on the condition, relative to others. This means it’s hard to know statistics but estimates run from 1-8%.
The number varies for multiple reasons:
It’s still unknown so medical professionals don't necessarily have the education needed to spot it, especially in general health.
There’s a lot of crossover with personality disorders, especially borderline personality disorder (Some people have posited that trauma exists on a spectrum, encompassing PTSD, cPTSD, BPD, and dissociative disorders such as DID). This can lead to people being mis-diagnosed, or not diagnosed at all, depending on their symptoms (BPD is massively stigmatised, and DID is often dismissed as not being real).
Then there’s general reasons people are dismissed:
People don’t have the words to explain their symptoms
We still don’t really see emotional abuse and neglect as ‘real’ abuse, especially one that can rise to causing a diagnosable condition
A lot of people struggle through because there’s such a high barrier to mental health services in general
Given the higher rates of self-harm and substance misuse, we tend to treat those rather than the underlying causes.
Most of the research on spotting and treating it has been done in children and adolescents. We know that certain experiences in childhood (Adverse Childhood Experiences) can affect mental health, as well as lead to increased levels of self harm, substance misuse, and sucide.
In a 2014 UK study on ACEs, 47% of people experienced at least one ACE with 9% of the population having 4+ ACES ().
I am one of the 9%.
The list is incomplete - most places say the 9 core ones are a starting point, not the entirety of things that can affect peope. Things like food scarcity, parentification*, emotional neglect can also lead to issues in adulthood.
*Parentification occurs when parents look to their children for emotional and/or practical support, rather than providing it. The child essentially becomes the caregiver. I was often my mother's therapist, hearing in great detail her relationship troubles, when I was a pre-teen, and right up until I cut contact.
On the other side of things, I once got teary after her partner insulted me. Her response was along the lines of me not mormally being bothered by his insults which is something terrible already. I replied I was stressed and this was the tipping point. Her response? How do you think that makes me feel, I should have known you were stressed, I'm a terrible mother. I didn't really tell my mother much, after that.
Treatment
Treatment for cPTSD is all about learning about your emotions and responses to stress, reframing problematic thought patterns, and exposure therapy where needed.
There is some evidence that trauma-focused CBT can help children and adolescents. This, alongside family therapy, is aimed at rebuilding a safe home life and relationships. There's little research into treating cPTSD in adults.
I had NHS CBT, which…didn’t really work, for multiple reasons.
It did a lot for the in the moment anxieties, giving me ways to gentle parent my brain essentially, but it didn’t start to unravel the underlying beliefs that fueled these thought patterns.
It also didn’t do anything somatic, I didn‘t really talk in depth about what I was feeling or how it felt. I was told to assign an arbitrary number to how anxious I was, but that was it.
Looking back, I’m not sure it would’ve worked when I was still in contact with my family. You can’t start undoing the patterns of trauma if they’re still being reinforced regularly and those survival techniques are still being used.
Self help: Mindfulness and yoga
I did mindfulness through the nhs for anxiety and chronic pain (there is evidence of correlation between trauma and chronic pain, and there are definitely some correlations in my life where my mental health affects my physical health).
Years of dissociation plus chronic pain meant I didn’t really have a relationship with myself mentally or physically, so mindfulness and yoga was a safe way for me to be in my body in the present.
It wasn’t enough.
I knew I needed to talk to someone in 2018, so I found a private therapist. I’d not heard of person centred counselling, and didn’t really do any research, I just went to an appointment.
I conencted with my therapist pretty much immediately. I can’t pinpoint a moment, other than we both swore in our first session, and I remember how important it was for me to hear him say that something I went through ‘sounded really shit’.
Having the space to work through my feelings and beliefs without homework or having to deal with people defending my family helped me have massive breakthroughs. I didn’t have to worry about trauma dumping, or someone pushing back against the words ‘abusive’ or trying to make me feel better. I could have whatever feelings I had.
Just being believed and taken at my word was a massive thing for me and allowed me to really dig into what I was feeling and why.
My therapist also challenges me, but only when I'm bullshitting myself.
I cut contact with my family a few months later, when it really hit home that I was never going to make real progress with my family in my life. It was a really difficult decision, and the best one I’ve ever made. I’ve written about the aftermath a bit here: Why I Cut Contact With My Biofam.
I’ve been in therapy pretty regularly ever since, unpacking and untangling my past. I’ve come a long way, but there’s still some way to go.
The Future
My current challenge is around personal safety. I find it difficult to trust safety that isn’t something I’ve built myself. So right now, in self-employment where I’m having to rely on my partner more than I’d like to financially. It’s difficult to feel safe when I’m not used to it.
In the research world, there's been some interesting studies, for example this study on PTSD and cPTSD in UK Firefighters.
There's still research being done on the inclusion of cPTSD in the ICD11, and what the diagnosis means. I'm hoping that as more people come to learn of the condition, the diagnosis, and healing from trauma, we'll get more insights into the varying ways trauma can manifest in a person.
cPTSD is a fundamental part of my life, and I've written before about accepting where I am in my journey.
I do think there'll be things that will always trigger me a little, or cause cPTSD symptoms. While I've come a long way, and still want to work on some things, others I'm happy to manage as needed.
My goal by writing this is to make people feel less alone, or get some insight into themselves. I hope I manage to educate some people about this condition that we don't really talk about.
Thanks if you managed to read it all! This is a free newsletter, so feel free to share and forward it to anyone who would appreciate it!
Add a comment: