I said in my previous post that we are going to start at the molecular level – and I really mean the most basic molecular level there is – and work our way up to the concept of reassortment today. Reassortment is in the news because another strain of avian influenza, H5N9, has just been detected on a duck farm in California. One possibility is that this H5N9 is the result of a “reassortment event,” which is a bad sign, although it doesn’t yet change the public health risk to humans (H5N1 and H5N9 are both avian flu viruses, which do not readily infect humans and can’t spread between humans). We will learn why this is and what all of this means by the end of this post.
But first, I’m going to start with some outdated high school-level biology. This is a paradigm called the “central dogma,” which was already crude and out of date by the time I learned it 20 years ago. I am mentioning it here for sheer pedagogical utility – I think it is the quickest way to bring everybody onto a level playing field with this stuff. So here we go. Living things are made of cells, and each cell contains genetic material. In humans, our genetic material is DNA. There is a similar molecule called RNA which makes up the genomes of some organisms, like influenza (is influenza “alive”? Sort of. We’ll see.). The central dogma that we were taught is that life functions occur via the twin processes of transcription and translation. The DNA encodes “instructions” in the form of codons or genes; this information is copied into so-called messenger or mRNA (transcription). Then the mRNA transcripts are “read” to assemble proteins and other macromolecules that do whatever the cell needs to do. As I’ve said, this is a hugely incomplete and simplified picture, but this is the basis for how we are going to understand what a virus does.
At the most abstract level, viruses work by getting into your cells and taking over (much popular science writing uses the term “hijacking”) this cellular machinery of transcription and translation; instead of making the macromolecules needed for whatever cellular function, though, the virus directs the machinery to just make more and more copies of itself. Those copies then bust out of the cell and find other host cells to infect, repeating the process over and over again. Viruses have genetic material, but little else – they are generally just some DNA or RNA wrapped up in a rudimentary membrane, as in this image:
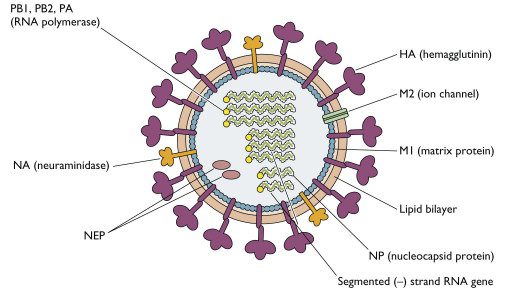
A couple of components to notice here. The first are the hemagglutinin (HA) and neuraminidase (NA) molecules on the membrane in the diagram. These are what the H and N nomenclature system refers to. In his 2005 book on avian flu, Mike Davis describes them thus: “if HA is the burglar, NA is the escape artist.” (p. 18) HA gets the influenza virus in to the host cell, NA gets it out. Note also the “RNA polymerase” components. RNA polymerase is the enzyme that effects the replication of influenza’s RNA genome. Humans have an analogue – DNA polymerase – that replicates our DNA genome when, for example, a cell divides. The thing to note here is that RNA polymerase is extremely error-prone. DNA polymerase has high copying fidelity, and makes few errors; if RNA polymerase were a typist (again borrowing a metaphor from Mike Davis), it would make a typo every couple of lines. This is important for evolutionary change of the influenza genome/influenza virus. Random mutations – errors in copying – provide the variation that natural selection works on. Combine this with how extremely short a viral “generation” is compared to a human one, and it’s not surprising that influenza viruses can evolve extremely quickly.
You’ve probably seen news articles about evidence that H5N1 has acquired such-and-such mutation that increases its ability to infect or replicate in mammalian cells. These are all talking about the first of of two tracks along which the influenza virus can change and (potentially) acquire pandemic potential: evolution. (The second is reassortment, which I will talk about next.) I’m going to cite extensively from a thorough recent review article by Peacock et al. (2025) (I love that this expert in avian flu has a bird-inflected last name). These authors outline the three preconditions for avian influenza (or any influenza virus, really) to become a pandemic. First, the HA component has to be “antigenically novel and poorly recognized immunologically by a large fraction of the human population” – meaning, essentially, that there hasn’t been widespread exposure to or vaccination against this HA component in the human population, that the human population are “naive” to it. (Mike Davis again: “Pandemic influenza is usually defined as the emergence or reappearance of an HA subtype against which most people have no prior immunity,” p. 14). This criterion is already met for H5, which has never circulated broadly in humans; few humans have been exposed to it, meaning very little population immunity. The second precondition concerns the stability of the HA component, which I won’t go into. The third and final precondition is the big one: the virus must change to be able to spread easily between human beings.
Let’s start with Mike Davis again: “HA’s success at breaking and entering is the sine qua non of an influenza infection” (p. 14) and, a few pages earlier:
While… HA is the molecular key that influenza uses to unlock and enter host cells, different key configurations are needed to open different cells. Avian influenza HA, for example, generally only unlocks the intestinal cells of waterfowl, while human HA has been refashioned to break into cells in the mucous lining of the respiratory system. This difference in lock and key configurations is generally considered to be the species barrier that prevents avian influenzas from easily circulating among mammals. (p. 12)
Mammalian cells of different species (humans, pigs, cows, etc.) are similar in many ways, but also very meaningfully different. (How’s that for a dumb-guy-trying-to-sound-smart phrase? It’s true, though. A lot of the molecular biology I learned in undergrad smooths over the differences that matter here in service of presenting abstracted general principles.) To help the virus get in to the cell, the viral HA molecule attaches to molecules on the surface of host cells containing something called “sialic acid receptors.” From Peacock et al. (2025): “These receptors come in different forms and have different distributions in birds, humans, and other mammalian species” – one form abounds in many bird tissues, cow mammary glands (more on this and the role of milking machinery in spreading H5N1 in cattle to follow), and in the human eye (note that many of the documented H5N1 infections in humans in this outbreak have involved conjunctivitis) and human lower respiratory tract (lungs). But to spread efficiently between humans (rather than from, say, cow to human), the virus has to bind to, enter, and replicate in the tissues in the upper respiratory tract (nose and throat), which are populated with a different form of the sialic acid receptor. Peacock et al. (2025) describe this as a major “evolutionary hurdle” that H5N1 and other strains of avian influenza would need to clear in order to go (airplane emoji) pandemic mode – to become a pandemic, influenza must spread readily between human beings, which H5N1 and other avian flu strains currently, thankfully, do not.
While mutations are frequent in the RNA polymerase component of the avian influenza virus (including mutations that allow it to make more efficient use of the host cellular machinery to synthesize more of itself), the mutation of the HA component appears to be, in evolutionary biology jargon, “constrained.” Mutations do not arise as readily there (possibly because it is more critical to the survival and propagation of the virus that some basic structure of the HA component be conserved) and, as Peacock et al. (2025) note, mutations haven’t arisen widely in this component during previous H5N1 outbreaks, including in ones where we might surmise there would be favorable selective pressure encouraging more efficient binding of the sialic acid receptors found in the upper respiratory tract.
So the news articles you see about mutations are cause for concern and for continued (increased!) monitoring, certainly, but change along this evolutionary track is gradual, it is random (and so highly unlikely to get all the mutations needed to transform H5N1 into a virus with pandemic potential “right”), and it appears to be evolutionarily constrained in some meaningful ways.
Unluckily for us, there’s a shortcut: reassortment. Influenza’s RNA genome is segmented. Reassortment essentially means two influenza viruses in close contact swapping entire segments of their genome. This is the really scary potential, that an avian influenza virus could acquire the stuff it needs to efficiently spread human-to-human all at once via reassortment. In order for reassortment to take place, a host cell (in a pig, a person, or whatever) has to be co-infected (infected at the same time) with two different strains of influenza. The nightmare scenario this flu season is a person, likely a farm worker, infected with a human-adapted strain of influenza A who also picks up H5N1 from infected cattle or poultry. That could set the stage for a very bad reassortment event. You always hear pigs mentioned as an ideal “mixing vessel” for flu – this is about reassortment. It’s because pigs are mammals that can be infected with a wide range of influenza viruses, avian, and mammalian, including human. Pigs are also factory-farmed, meaning that they live in conditions that are, shall we say, favorable to promoting the spread of infections of all kinds, and potentially fairly exposed to other domesticated or wild animals. Reassortment is where the rubber hits the road in terms of really risky changes that could send us careening into the next pandemic. Again from the Peacock et al. article that I have been extensively quoting:
A farm worker coinfected with H5N1 and a human seasonal virus presents an opportunity for avian and human IAVs [influenza A viruses] to reassort and combine many of the traits needed to spread efficiently in humans, as occurred prior to the 1957 H2N2 and 1968 H3N2 pandemics. H5N1 spillover into swine… would present additional opportunities for reassortment, as exemplified by the triple-reassortant swine-origin H1N1 pandemic from 2009… The continued absence of H5N1 in US swine is highly fortunate.
Considerations about reassortment quickly telescope into questions about social and economic conditions, farming practices, labor conditions, ecological movements and adjustments, and so on. These will be the subjects – broadly speaking – of the posts in this series to follow. I hope that having a little bit of an explainer on some of the science can help you make sense of what you’re encountering out there in the slop information environment.
A few things I want to mention before signing off. First of all, the Sick Times updated their informational materials to clarify the mechanism of H5N1 spread after my newsletter back in December, and I’m overdue in giving them daps for this. Love to see it. I’m sure their newsroom is under extreme stress right now with everything going on federally, so if you’re looking for (and/or to support) independent health journalism, check them out. Second, as we will see in subsequent posts, the path forward in terms of what we ought to be doing about the H5N1 panzootic is extremely complex (and I don’t know the answer), but I want to emphasize the importance of focusing on occupational health and safety and on conditions for farm workers. A recent NYT article, for example, noted that human H5N1 infections have certainly been missed because undocumented farm workers are afraid to seek testing for fear of being deported. There’s a whole other post in here about public health and the “worldedness” of the biopolitical interventions we study in isolation – how, as I said on cursed Bluesky, ideologically neutral public health practice can actually function to render people visible to a hostile state. I don’t have an answer here, other than to keep farm workers at the center of whatever advocacy you might be doing around this. For example, a mask bloc in my area is currently organizing materials to distribute directly to farm workers in the state, both educational materials and also literal PPE like gloves and goggles. (I think goggles are particularly important given the apparent susceptibility of the eyes to H5N1.) Doing it on a grassroots mutual aid basis is not ideal, but equipping workers with PPE has the potential to prevent spillovers (human infections) which can lead to reassortment.
Till next time.
You just read issue #62 of Closed Form. You can also browse the full archives of this newsletter.
