All’s well that ends well.
But endings are hard.
alright wrap it up, we're done, idk how we're gonna top this one pic.twitter.com/8w0Ndly7nb
— mr pussy (@mrpxssy) December 13, 2025
The meme mocking the right’s attempts to make Charlie Kirk into a martyr has gone viral, and is now spreading at our kids’ school, right alongside “6-7”.
(The song used by the meme was itself AI slop. It’s lazy grifters all the way down.)
Why are the kids all in?
It turns out that young people pay close attention to what people actually say (i.e., “counting or not counting gang violence”), and they think it’s more than a little ironic that a person who justified school shootings for a living got killed in one.
(Our boys had three active shooter drills this Fall. They talked in the days after of where they would hide from a killer with an assault rifle.)
While fascists and other grifters often use sensational, violent deaths to advance their politics, it’s the mundane, every day deaths that should dictate where our attention lies.
Specifically, the “normal” deaths that awaits millions of Americans: solitary, poor, nasty, brutish, and long.
Nothing good happens when people look the other way.
We spend a lot of time talking about the start of our lives, from celebrating birthdays to using “baby” as a term of endearment.
By comparison, we spend very little time talking about the end of our lives.
It’s a curious blindspot since most of us would agree that the ending of the story is what gives it meaning.
Closure, as it were.
Some people have asked me if I’ve had time to heal from my mother’s passing but I had the fortune of her unexpected death.
One week she was giving me a recipe, the next week I was watching her gasp and then disappear.
That’s what we’d call a storybook ending.
For many, if not most, the process of dying, the story of dying, unfolds quite differently.
For example, shortly after my mother died, my father fell.
Then he fell again, and again, and again, and again, and again, and again, and again, and again, and again, and again, and again, and again, and again, and again, and again, and in doing so, he has begun to die, as well. Albeit very slowly.

This pacing will be very familiar to some of my older readers.
Yet it’s largely absent from the popular imagination where dying is either an exclamation mark or a goof.
e.g., pointing a finger gun to one’s head is a joke because dying is understood as a form of relief.
To joke – or even imagine – one’s own sudden death is a fantasy precisely because in real life dying is seldom quick or clean.
It’s slow. And messy. And hard.
And that, my friends, is why we ignore dying.
Dying requires a great deal of care.
Attention must be given to a person who is never going to produce anything again and that is a bridge too far in our society.
Caring is how we give importance and we don’t give importance to those who aren’t productive.
Children, for all their heavy diapers, are going to eventually do something for us. But the elderly are an inverse: we must do something for them, and get nothing in return.
“Why should we care?” infects “how we care” so fundamentally it degrades and destroys everything that touches our dying.
Health, Care
On many occasions in the last two months, my interactions with hospitals as they provide “care” to my father has nearly broken me.
I had written an entire newsletter about these experiences, mostly from my father’s bedside, but they can be boiled down to a short list:
The hospital is not a place where people are healed.
The hospital is a set of discrete procedures, each prescribed by a specialist.
The doctor assigned with the task of integrating and synthesizing these interventions is not expected to know events prior to the hospitalization. Whatever cannot be gleaned via a machine – whatever knowledge comes from relatives, etc – is supplementary.
When the hospital does not produce a unified story about the patient’s past, present and thus future, the care being given is mechanistic, not humanistic.
The hospital may effectively treat discrete symptoms, and even causes, but it also dehumanizes its subjects. The human is lost in the (sterile) sauce.
This dehumanizing treatment is especially dangerous for people with the human condition known as “the process of dying.”
What is a human being?
A set of stories. That’s literally what we are.1
What we need to become human, to remain human, is stories.
Perhaps, if you’re lucky, you’ll go to a hospital one day and the protocols will find a biological process they can describe to you: “your heart is beating too fast”, “your stomach has an ulcer”, “your leg is broken”.
Such has not been my fortune with my parents’ hospital stays. And I suspect my experience is typical for anyone who goes to the hospital for the condition called “dying.”
Dying, it turns out, is often multifactorial and as such there is no one treatment for it. And that’s where the hospital, as a place that is intended to improve our lives, fails entirely.
It can’t synthesize. It can’t coordinate. It can’t care for the human as a whole.
In this way, the hospital fails entirely those who are dying which, in reality, means it fails to heal. Because dying is not an injury, a wound, a malfunction; dying is as much a part of life as being born.
But unlike gestation, dying does not have a consistent or even knowable duration.
9 months? 6 years? Three weeks? Who knows!
Which, in turn, leads to “who cares”?
Why did my father fall 16 times in four months?
After treating his external wounds and running a series of quick tests – CT, MRI, ultrasound – the hospital concluded: we don’t know. Find someone who does. “Try Yelp.” (Direct quote.)
The only thing the hospital went out of their way to find out was the margin on his care; revenue minus cost.
I am certain of this because no doctor ever called me to tell me anything. Instead, I had to arrive at 6am and leave at 9pm in the hopes that I might be so lucky as to see a doctor to whom I could relay my father’s medical history so that they might adjust their treatment plan accordingly.2
No, the hospital only ever called me, repeatedly, almost hourly, when they wanted to discharge him to a facility.
And perhaps receive a kickback for doing so. After I passed on one such facility, they sent the business development person from that facility to my 84 y.o. father’s room to pitch me again.
Did they send anyone to talk about his emotional wellbeing? His goals in life? Ours?
LOL.
Coda
Of course, the language of the hospital is dominated by acronyms like PCP, for Primary Care Provider (fka “family doctor”), and, in our case, SNF’s, for Skilled Nursing Facilities.
When my father was first discharged on Thanksgiving day, he was sent to a skilled nursing facility. I went with him in the ambulance expecting some continuation of the care he had received at the hospital. Instead, we found a dingy warehouse of bruised elderly bodies, three in a room, each with their own television, the hallways crammed with shouts.
After 45 minutes of panic, I signed the paperwork to release him to our home. I slept that night in the La-Z-Boy next to his bed.
Two weeks later, after he had recuperated most of his strength, he fell and drew blood again, this time breaking a tiny piece of a neck bone.
You might think we’re just having bad luck but in fact it was just a lot of luck: because that very same day my father had an appointment with a neurologist. It was an appointment that I’d first made in July when he moved to California but the doctor’s next availability was months later. Alas, we’d had to reschedule the first appointment when my father was hospitalized the first time. And now I was calling to reschedule it again because of another fall.
When would this brain doctor finally be able to see my father who had fallen 16 times? Three months later? Really?
Well, it turns out this doctor happens to make the rounds at the hospital and he walked into the ER room for my father’s first consult.
But while this doctor could begin to change my father’s psychotropic medicines, there was no immediate way to prevent him from falling again. That would require “care”.
This time around, I knew that finding a decent SNF would be hard so I started the search on day one. Sixteen were contacted, including more than one that would have required out of pocket pay – about a third of my father’s meagre savings for a month of rehabilitation.
Yet none – not a single one – could either accept his (“good”) insurance or provide him with the isolation he needs as a person with PTSD.
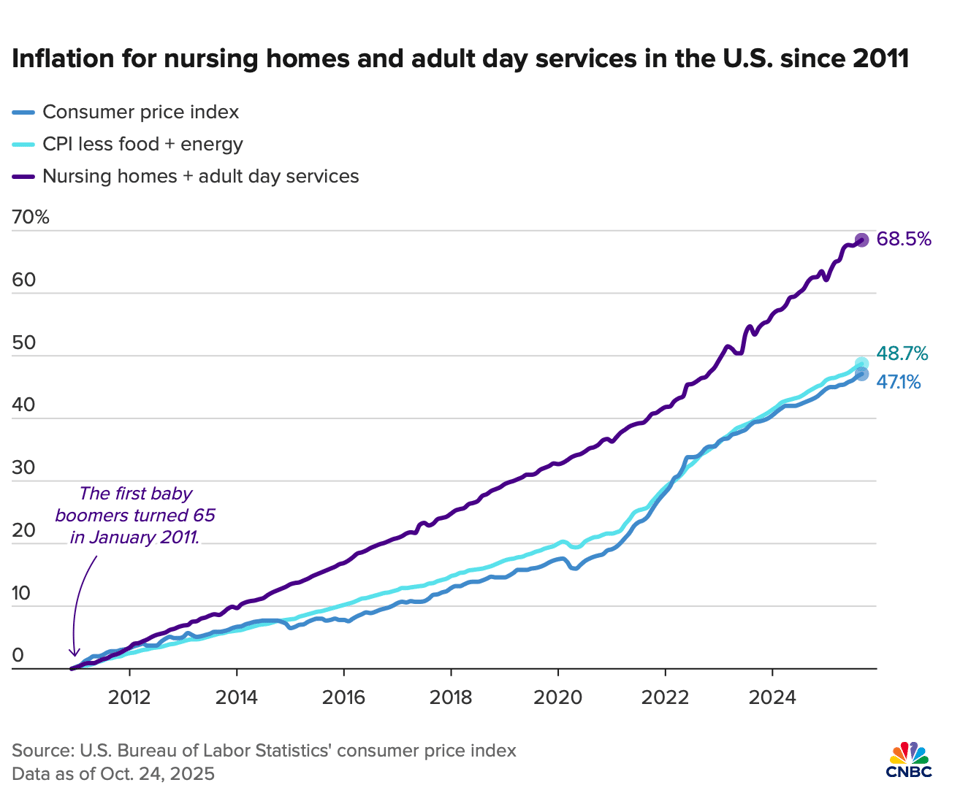
For sure, the housing crisis is much to blame. But here it intersects with a broader problem.
Because we would prefer not to think about dying, because the old have no productive value, because we do not value care, because we do not fully understand what it means to be human – or would prefer to forget, as remembering requires us to care – there are no places where people can go to ease into their endings.
Pull on that thread…
Perhaps, it will come as no surprise that this denial of our material reality, and of who bears its burdens, begins at birth…
