Saturday, July 22,2023. Annette’s News Roundup.
I think the Roundup makes people feel not so alone.
To read an article excerpted in this Roundup, click on its blue title. Each “blue” article is hyperlinked so you can read the whole article.
Please feel free to share.
Invite at least one other person to subscribe today! buttondown.email/AnnettesNewsRoundup
_________________________
It will be a light Roundup weekend. I hope you don’t mind and, hope that, like me, you are enjoying a few days kind-of-off.
Here, though, is an article I found important. It provides information worth putting in a file, to access. Keep Dr. Saud Sadiq and the Tisch Center in mind if you or someone you know may have M.S.
A New Approach to M.S. Could Transform Treatment of Other Diseases
Multiple sclerosis was once seen as a “dead-end disease.” But lots of little interventions have added up to remarkable progress. Should that change how we take on other conditions?

In 2014, Erin Storch looked in the mirror and felt as if she were drifting leftward. It was a feeling she didn’t know how to fully describe. She had been on maternity leave, and had recently returned to her job at a hospital consultancy in Washington, D.C. Storch had been promoted while on leave, so she was learning something new at work—and it seemed strangely difficult to absorb the information. She was also pumping milk three times a day. People suggested that what she was experiencing might be profound exhaustion; she disagreed. “I knew in my gut that the way I was feeling was not within the spectrum of what you would consider normal,” she said.
There were further unsettling sensations: “Coffee tasted like water. The left side of my body was weak and numb.” Storch went to see her ob-gyn, who sent her for a CT scan. Nothing unusual showed up.
Storch’s son was six months old when her symptoms manifested. When he was seven and a half months old, she walked down the stairs while holding him, and fell. Her son was O.K. “But then I knew that something was really wrong,” she said. She found a new doctor, who sat with her and her husband “for maybe forty minutes. It was just a conversation—there wasn’t even a physical exam. He said to me that he knew a lot of moms with demanding careers and that this was not that.” She started to cry from the relief of being believed. He scheduled an MRI for that evening. “But since there was some time to kill I decided, being me, to go to work,” she said. She crashed her car into a pole in a garage on M Street.
The MRI showed that Storch had several lesions, indicative of inflammation, in her brain. She was admitted to the hospital the next morning, where she was eventually told that she had multiple sclerosis, a chronic disease characterized by inflammation in the brain and the spinal cord. While Storch was in the hospital, her mother and her sister used breast milk from the freezer to feed her son, who had never had formula.
Despite her diagnosis, there was little clarity. In the hospital, she recalled, there was one doctor who, in response to her husband’s questions, replied, “Have you heard of Google?” (Storch says that she did go down “a Google rabbit hole, and I didn’t find anything that helped me.”)
After Storch went home, she started seeing a neurologist, who, she said, “was doing the best with the tools they had—this was not an M.S. specialist.” The neurologist put her on a pill that had recently been approved by the F.D.A. She began seeing a psychotherapist, too. “She wanted me to educate her on the disease,” Storch said. “She would ask questions like ‘Is it possible that you could be in a wheelchair?’ ” Storch realized that she didn’t know. Also, the medication she was taking didn’t seem to be helping.
Around that time, Storch received an e-mail from someone she knew at work, recommending a doctor. “That was how I found Dr. Sadiq,” Storch said.
Saud Sadiq is the director and chief research scientist of the Tisch Multiple Sclerosis Research Center of New York and the head of the adjacent clinical practice. Speaking with his patients can feel like speaking with devotees of one of those bands which border on being a religion. Patients told me that he talked with them until they ran out of questions, that he saw them on a Saturday so they could have their normal life, that he gave them his cell-phone number. Amelia Collins, who has been his patient for twenty-three years, told me that she once heard his cell phone ring while he was performing a spinal tap. He said to her, “You see, this is the only time I won’t answer my phone, because I have your spine in my hands—otherwise I would answer.”
Storch said, “We sat in his office, and everything that I thought a health-care experience should be—that was what it was. It felt like he had unlimited time.”
There are two main types of M.S.: a relapsing-remitting form (R.R.M.S.) and a progressive form. Both attack the brain and the spinal cord and can become debilitating if not treated, but R.R.M.S. usually responds well to current therapies. The progressive form, which often presents as what is called the primary-progressive type (P.P.M.S.), which affects about fifteen per cent of patients, tends not to. As their names suggest, R.R.M.S. is characterized by symptoms that flare up and then often spontaneously remit, and P.P.M.S. proceeds more inexorably. Sadiq told Storch that she likely had R.R.M.S., and advised her that an aggressive course of treatment could stave off further disability. Once damage is done, it is often irreversible. He told her that the medication she was taking may as well have been a water pill.
Sadiq told Storch that she would have no more disease progression, and, she said, “that has been the case.” She takes a drug, Ocrevus, that eliminates her B cells, an element of the immune system which, in M.S. patients, attacks the nervous system. Her Ocrevus infusions, given twice a year, are accompanied by an infusion of steroids. “I know that knocks me out for a couple days, so I plan on that,” she said. “I save a bad TV show to watch.” She also takes two medications that help with symptoms: gabapentin for numbness and tingling, and modafinil for fatigue. “I used to call the office so often, but now M.S. is less at the forefront of my life. It’s just something I manage like I manage everything else,” she told me. Storch struck me as professional, reserved, and put-together. She teared up only once, when she said she didn’t know what her life would be like today if she hadn’t met Sadiq.
I recently spent a couple of stressful months trying to get appointments for a close relative with a newly diagnosed neurodegenerative disease—appointments with neurologists and ophthalmologists and neuro-ophthalmologists and radiologists—and trying to find, as several of the neurologists suggested, a way to get an appointment with the right kind of neurologist. I often wished there were a practice organized like Sadiq’s, with all the players in one house, and clinical trials as well as basic scientific research happening there, too, where the researchers’ ambitions were influenced by the problems seen each day. “It happened not by careful thought but because, when I was the chairman of neurology at St. Luke’s-Roosevelt, I was frustrated with the bureaucracy, and the bureaucracy getting in the way of the research, so I decided to open an independent lab and practice,” Sadiq told me, when I visited the center not long ago. “If I had thought about it, I wouldn’t have done it, because there was no prototype to copy. In hindsight, it was unlikely to be successful.” Sadiq was especially eager to show me the backup ventilation system for the animal-care area—it was so large that it had to be installed through the windows. “If we want to do creative and innovative research—that’s very difficult to do when you’re under pressure to publish or secure more funding,” he said, explaining why he valued working outside a research hospital like those in which he trained.
The approach of housing all M.S. services together, as at Sadiq’s practice, can seem less than revolutionary, but at a recent “patients as teachers” session at the Barlo Multiple Sclerosis Center, at St. Michael’s Hospital, in Toronto, the patients spoke about the value of having care from different providers be coördinated. Providers want this, too—it is sometimes called comprehensive care—but the usual demons of funding and structural change are difficult to overcome. Even the Barlo center, a strong model for comprehensive care, is described by its director, Jiwon Oh, as “still a work in progress.”
Sadiq is gently boastful of how his center functions. “I saw a patient yesterday who was seen at an Ivy League M.S. center, and they told her she needed another MRI but couldn’t schedule it until two weeks later,” he told me, “and her treatment couldn’t start for another three weeks after that. When she came to see me yesterday, because we have two MRI facilities downstairs, we did it immediately and she’s starting treatment tomorrow.” A popular saying in the treatment of strokes is “Time is brain”—it’s important to get a clot dissolved as soon as possible. Today, with M.S., there is a similar emphasis on early treatment, since time is both brain and spinal cord. “She is going to get married in November, and I want her to have a good wedding, walk down the aisle,” Sadiq said.
Sadiq, who is sixty-eight, is fond of describing himself as a “very boring-in-general guy,” and “just an old man working” who occasionally attends a Yankees game. “But I am too busy, so mostly I give my tickets away,” he added. His wife died of ovarian cancer last year, and his son is in his thirties. Sadiq lives in New Jersey with his mother, who is a healthy ninety. “This is my dream, I love what I do, my life is this,” he said of his research and clinical practice. He feels that he has “limited time,” and told me, “I hope to find these things”—better treatments for M.S.—“quickly.”
Sadiq was born in Kenya, and graduated from the University of Nairobi’s medical school in 1979. He did his residency in internal medicine in Kenya and in the U.K. between 1981 and 1985, and so has witnessed the arc of how dramatically M.S. outcomes have changed in the past half century. “When I was in school, and in residency, M.S. was a dead-end disease. It overwhelmingly led to disability,” he told me in his office, which is decorated with model ships, Yankees paraphernalia, illuminated Torah passages, golden Virgin Mary icons, and other gifts he has received during his decades as a neurologist. The patient was often a young woman, since M.S. affects women three times as often as men and tends to present in a person’s twenties or thirties. Part of the terror of M.S. was not knowing when an attack—which might manifest as a loss of sensation, or a loss of vision, or a loss of strength, or any other number of troubling losses—would come. Patients were not unlikely to end up confined to a wheelchair, or to have a sense of pressure on their chest, a dread of warm days, trouble seeing or blindness, or difficulty controlling their bladder and bowel movements; sometimes holding a pencil was a challenge. “If the patient was young, you would not tell her about her prognosis for as long as you could,” Sadiq said. “That seems crazy to me now. But that was what was done. You told the parents or the spouse, but not the patient.”
In 1985, Sadiq moved to Galveston, for a residency in neurology at the University of Texas. It was, he said, “the year after MRIs came into widespread clinical use.” MRIs are now commonplace, but they’re still astonishing: after you’re slid into an MRI machine, all the water molecules in your body orient themselves along the lines of a magnetic field, as if saluting; radio energy is then pulsed through the body, which stimulates the protons of those water molecules to varying degrees, depending on the part of the body. MRIs are thus particularly good at imaging soft tissues, such as muscles, abdominal organs, and the brain, where the lesions typical of M.S. show up. “Previously, you were working with subjective complaints,” Sadiq explained. “Now you could objectively characterize the lesions.” In early years, MRIs were used only for diagnosis, because the machines were rare; now they’re also used to monitor disease progression.
MRI imaging is not just about helping a doctor “believe” a patient’s story, or giving a patient the validating feeling of “seeing” her illness—it also opens up research possibilities, by enabling physicians to share a common language that is quantitative and transmissible (if still limited, since MRIs are just fancy pictures, and cannot explain all that a patient experiences). Whereas the move to make more room for a patient’s subjective experience helps in individual cases, the ability to speak both generally and precisely helps when thinking of a disease across thousands, or hundreds of thousands, of cases. If you were to think of the research trajectory of M.S. as a nineteenth-century novel, then the arrival of the MRI would be a decisive plot turn; in the data-mining storytelling of the twenty-first century, the change comes from the networks of thousands of patients and researchers coördinating and building up a body of knowledge bit by bit.
Multiple sclerosis presents far more variously than most other illnesses; for that reason, it has been called “the great imitator.” Some of the conditions it can resemble are minor, and others are major. If you have ever Googled a random tingling or twinge or eyebrow twitch, you have probably spent at least one evening convinced that you have M.S. On the other hand, M.S. patients often think for a while that they don’t have much going on. One person’s first symptom might be numbness. A different patient might experience weakness. Or an unexplained fall, or fatigue, or difficulty urinating or walking. In the United States, the incidence is around three people in a thousand, which is either rare or common, depending on the emotional heft you ascribe to a third of one per cent of the population.
Until recently, patients weren’t given medication before they were in distress; now treatment tends to come early, with the highest-efficacy drugs available. Oh, of the Barlo center, told me, “When I went into neurology residency”—in 2005—“the field was still sometimes called ‘diagnose and adios,’ because it seemed like there was so little that could be done for patients with these chronic neurological diseases,” such as M.S., Parkinson’s, A.L.S., and Alzheimer’s. “M.S. is the only chronic neurological disease where there’s been a very dramatic change.” In 1993, there were no approved M.S.-specific drug therapies; now there are more than twenty. Some treatments broadly target a patient’s immune response, and others interfere with the production of particular elements of the immune response which attack the patient’s nervous system. A study from Turkey comparing the records of an M.S. clinic in 1996 with those at the same clinic twenty years later showed a dramatic decline in the number of wheelchair-dependent patients—a particularly visible measure of disease.
When I spoke with Oh, she had been asked to address an A.L.S. conference, so that A.L.S. researchers might learn from the M.S. community. I asked her what she thought accounted for the progress; she talked about how visible the disease is, especially because it most often hits young people. “I don’t want that to sound ageist,” she said. It’s not unusual to know someone for whom the course of family and work life has been remarkably altered by M.S.; that attracts funding. Oh’s center raised twenty-one million dollars for its launch, which her hospital matched. The facility, which treats nine thousand patients, has expanded from four clinic rooms to twenty; its research and clinical arms are now on adjacent floors, and physical therapy, occupational therapy, and social work are also integrated into the space.
Jeffrey Cohen, the director of experimental therapeutics at the Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research, said, “The field does seem to be a little more organized. We have a well-developed set of diagnostic criteria, and a well-developed methodology for testing treatments and deciding whether they work. But another part of it may be that success begets success.” When something goes well, funding tends to come your way to do more such work.
For centuries, the treatment of M.S. hardly advanced at all. In the fourteenth century, a physician wrote of a Dutch woman named Lidwina of Schiedam, “Believe me there is no cure for this illness, it comes directly from God.” Lidwina’s is one of the first documented instances of what was most likely multiple sclerosis. Her illness, at the time, was attributed not only to God but to a fall while ice skating; she is said to have celebrated her paralysis and pain as an offering to Him, and she is now the patron saint of ice skating. People tried to ameliorate M.S. with leeches, quinine, foxglove, tobacco, hemlock, valerian, coffee, tea, being suspended above the ground, vertically, for four minutes at a time, and being wrapped in sheets sprayed with cold water. The nineteenth-century German poet Heinrich Heine (“There are two kinds of rat / The hungry and the fat”) did not know what he was suffering from when he wrote to a friend, “My legs are like cotton and I am carried about like a child. . . . My right hand is beginning to wither and God knows whether I shall ever be able to write to you again. Dictation is painful because of my paralyzed jaw. My blindness is still the last of my ills.” Heine, who died at fifty-eight, had a gash on his neck, inflicted deliberately, to which various ointments were administered.
The underlying causes of the symptoms of M.S. began to be gleaned with the work of the nineteenth-century French physician Jean-Martin Charcot, who is today considered a founder of modern neurology. The son and the grandson of carriage-makers, and the oldest of four brothers, Charcot was chosen by his father as the child who would get a costly advanced education. He studied medicine at the University of Paris. His brothers kept his study cozy with a hot cannon ball resting in a bucket of sand. Upon becoming a physician, Charcot took a position at the Salpêtrière Hospital, an old ammunitions factory that had been turned into, in his words, a “great asylum (of human misery).”
Salpêtrière held some five thousand patients. They were affected by chronic diseases of many kinds, but especially those of the nervous system. “We are, in other words, in possession of some sort of museum of living pathology of great resources,” Charcot wrote. His great scientific move can seem, in retrospect, ordinary. He set about differentiating and classifying, by symptoms, the residents of Salpêtrière, and then following them over time—including after their deaths, by studying their cadavers.
One case in particular focussed his attention on the destruction he saw in the brains and the spinal cords of certain cadavers. Charcot had hired as a maid a woman named Luc, who had motor difficulties. Charcot noticed that Luc’s tremors worsened when she moved about, and subsided when she was at rest—a different pattern from that found in Parkinson’s. (Charcot, with his colleague Alfred Vulpian, was the first to distinguish the diseases.) Luc broke quite a few dishes. As her symptoms worsened, she had to be admitted to Salpêtrière. Did she have neurosyphilis? A tumor? When she died, in 1866, he studied her brain and her spinal cord. He saw what he called sclérose en plaque disseminée. His drawings of these lesions as he saw them under a microscope show droplets of myelin—the sheathing around a nerve—floating free from the axon, the body of the nerve. Charcot was a gifted artist, and often said that what made a good physician was the ability to see without preconceptions. We now understand that many of the varied symptoms of M.S. occur when the myelin around the axon frays. An analogy sometimes given is that the nervous system is like the wiring of a lamp, and the myelin like the wiring’s protective sheath; when that sheath wears away, so much can go wrong.
In 1868, Charcot gave a series of lectures on the condition, which remain the origin story for the field today. He said that he did not know the cause of the disease; that it was most common in females; that the symptoms were intermittent and could spontaneously improve and then worsen again; and that “the prognosis has hitherto been of the gloomiest.”
The physician T. Jock Murray, a specialist at Dalhousie University, in Nova Scotia, in his comprehensive book “Multiple Sclerosis: The History of a Disease,” from 2005, writes about how theories of the causes of M.S. have shifted in parallel with trends in medical science: “In the era of Pasteur”—the father of germ theory—“it seemed to be an infectious disease; in the era of environmental illness, it seemed a disease due to some toxin; when epidemiological techniques flourished, interest centered on mysterious demographic and environmental factors; as immunology flourished, it became an immunological disease, and in this age of genetics, gene probes, and the human genome, there is great interest in a genetic factor.” This makes it sound as if each theory were later debunked, but Murray explains that the process of discovery was in reality cumulative. Cohen, of the Cleveland Clinic, summed up the current understanding: “Ultimately, we don’t know the cause, but it’s generally the same as I was taught in medical school—some genetic predisposition to an autoimmune condition, and superimposed on that are some environmental factors, including infection, that either trigger the process or play an ongoing role.” Some research points to the Epstein-Barr virus, which virtually all M.S. patients have; yet it’s been estimated that more than ninety per cent of the general population has it, too.
“There have been many times where the field has undergone a paradigm shift in terms of what we think is important,” Oh, of the Barlo center, told me. Currently, the shift is toward trying to better understand the progressive aspects of the disease, and why it gets worse over time. Oh said, “Now we feel we really have gotten ahold of the acute inflammatory component”—the flare-ups that characterize R.R.M.S.—“and so that’s made it apparent that it’s the progressive component of the disease that we don’t really understand.” Oh is a lead researcher on a prospective study following a thousand M.S. patients in an effort to identify factors that cause progression.
Medical research is a strange salad of astonishing, horrifying, life-saving, intriguing, confusing, even sometimes boring activities. Charcot refused to experiment on animals, and famously had on his office door a sign that read “Vous ne trouverez pas une clinique des chiens chez moi” (“You won’t find a dog clinic here”). What kind of research methods are being used today?
Several papers that emerged recently from lab research at Sadiq’s center make this question vivid. Jamie Wong, a neuroscience researcher, was a lead author of a paper in Brain, published in February, which examined a number of antibodies found in the spinal fluid of P.P.M.S. patients. Wong had injected the spinal fluid of those patients into the spinal sac of mice, and determined that this provoked P.P.M.S.-like symptoms—weakness, in this case—in the animals. (The strength of the mice is measured by having them hold on to the tiny silver bar of a grip-testing machine.) When the antibodies were removed from patients’ spinal fluid prior to its injection into the mice, the animals showed no symptoms of M.S. Of the many small advances that lead to interventions, this was a pretty big one.
Wong’s background is in spinal-cord injury. She came to the center’s lab because she wanted to do work that was integrated with a clinical practice—she meets patients. “That reminds me why I’m doing this research,” she said.
At the time that Wong was performing her mouse studies, Sadiq was recruiting Nicolas Daviaud, a French neuroscientist, who then began an organoid research project at the center’s lab. Organoids are the almost impossibly strange thing you might guess they are: tiny organs, not connected to bodies, grown, sometimes in clusters of ninety-six, in what look like doll-house ice trays. Since M.S. is a disease of the central nervous system, the relevant organoid for research is a brain. Daviaud grows miniature brains, each of which bears the DNA of a patient. He and other researchers can then study how M.S. progresses differently—which neural tissue is affected, and when—according to an individual’s genetic background, using these miniature brains.
Or, sort of brains. I spoke with Madeline Lancaster, a developmental biologist who runs a team at the M.R.C. Laboratory of Molecular Biology and who developed cerebral organoids. “They are not really brains—they are simplified brain tissues,” she said. She brought out some preserved cerebral organoids that she keeps in her purse to help people understand what they are. Their containers looked like dice for playing Dungeons & Dragons. She observed that, unlike a human brain, which has one cerebral cortex, an organoid can have more than twelve—but that it still has three layers of neural tissue around a fluid-filled ventricle, like a developing human brain. I asked—of course I did—if she worried that the organoids might achieve consciousness. She was patient. She said, “It’s hard to define consciousness, but it’s relatively easy to say what some of the prerequisites are.” She mentioned needing neural connections between parts of the brain, as well as a way for information to get into the brain and out of it: “An animal that can’t interact with its environment but that can still see—functionally it’s blind.” Basically, a brain needs a body.
Daviaud has a similarly untroubled relationship to the cerebral organoids he has nourished and grown. He explained his process to me: he takes hematopoietic stem cells, which we all have in our blood, and helps them multiply, then reprograms them into pluripotent stem cells, which are able to become any kind of cell at all. You may remember the controversy around whether researchers should be allowed to use stem cells from unwanted embryos. What few people seem to know is that this ethical conundrum was circumvented when a Japanese researcher named Shinya Yamanaka found a way to turn any old cell—hair, skin, blood—into a cell that, like an embryonic stem cell, can become almost any other kind of cell. (He was awarded the Nobel Prize for this work.) The process is “surprisingly simple,” Daviaud said. He grows the organoids for about forty-five days, at which point they are a few millimetres in diameter.
Sadiq and Daviaud intend to use cerebral organoids to try to answer a number of questions, including how the Epstein-Barr virus affects neural tissue. Scientists also believe that organoids might be used to test drugs directly on human nervous tissue, and to produce spinal fluid or other cells that might be useful in therapies. “But we have so much we’d need to know before then, like what if these cells keep developing and become cancers?” Sadiq said.
M.S. researchers have also begun to dream about actually repairing damage from the disease. Several early-stage clinical trials in the U.S. are exploring the use of mesenchymal stem cells, modified in the lab and injected into the spinal fluid of patients with progressive forms of M.S., in the hope of reversing the disease’s progression. Lauren Louth, a forty-four-year-old nurse, recently participated in a two-year clinical trial at Sadiq’s center that was based on work by the researcher Violaine Harris, who has been affiliated with the center since its founding. The trial had what is called a compassionate crossover structure: half the patients received the stem-cell injections while the other half received a placebo; then, after a year, the treatments were switched, so that all the patients had access to the potential treatment. Louth first learned of her M.S. when she was working in an emergency room in 2005; she remembers looking at a patient and seeing double. She mentioned this to the doctor she was working with, and received an MRI and a probable diagnosis before her shift was over. “I told my fiancé, ‘The wedding is cancelled, we’re not getting married, you’re not changing my diapers,’ ” she said. (She is now married to that fiancé and has two kids.)
Her symptoms worsened over time. Walking became difficult, her cognition declined, and she experienced a tightness known as an “M.S. hug.” She lost some dexterity in her left hand, which is her dominant hand. “I would wake up and feel so heavy-headed, thinking, What will I lose today?” she said. She lived with the disease, sometimes taking medications for it and sometimes not, for many years. Then, in a particularly low moment, she travelled from her home in Rhode Island to see Sadiq, whom she had not met before. She wanted to ask his opinion about stem-cell therapies.
Louth ended up being Patient 48 in the stem-cell trial run by Sadiq’s center. On paper, only small benefits over the placebo were seen, and only in patient groups with higher disability scores; for that subgroup, walking times improved, and also bladder function. Louth told me about her subjective experience of the treatment: “I feel sharper. That brain fog, that feeling of flightiness, where you’re everywhere but where you’re supposed to be”—she felt that it had lifted, and that her heat intolerance became “pretty much nonexistent.” For the first time in a long time, she enjoyed rather than feared summer. Many doctors and patients say that the more difficult-to-measure symptoms—those that affect mood or cognitive function—are more important. Oh said that they are sometimes termed “silent symptoms,” but “they are not at all silent for patients.”
After the stem-cell trial, Louth “started having stability of symptoms,” she said. “I don’t wake up every morning thinking about what I will lose.” Subjective reports are both more and less reliable than objective ones, in that they capture hope and happiness, and the state of our inner lives, which most humans agree are among the highest priorities.
Sadiq isn’t all reason and numbers. Louth recalled that he told her he had prayed that he would be able to help her. Different emotional narratives coalesce around different diseases: it is not unusual to think of cancer as an invader; to think of autoimmune diseases as a betrayal of self; to think of neurological diseases as a sort of ghost or a supernatural takeover. It’s not surprising, in that narrative, to learn that Charcot tried to hypnotize patients who had been diagnosed as hysterics. He held Tuesday-afternoon demonstrations, equipped with theatre lighting and a stage, which were akin to exorcisms. His most famous patient, Blanche Wittman, would go onstage and, in front of an audience that sometimes included Guy de Maupassant and Degas, cower as if seeing a snake, or bark orders as if directing troops—and then later have no memory of these acts. Some of Charcot’s colleagues were appalled by the scenes, which they saw as a return to the pseudoscience of mesmerism. Charcot himself was also disturbed. That humans were so suggestible seemed like something science would need to account for. “In the last analysis, we see only what we are ready to see, what we have been taught to see,” Charcot, the teacher of Sigmund Freud, said. After Charcot died, of heart disease that he had self-diagnosed, Blanche Wittman never had an attack of hysteria again. ♦ (New Yorker, By Rivka Galchen).
_________________________
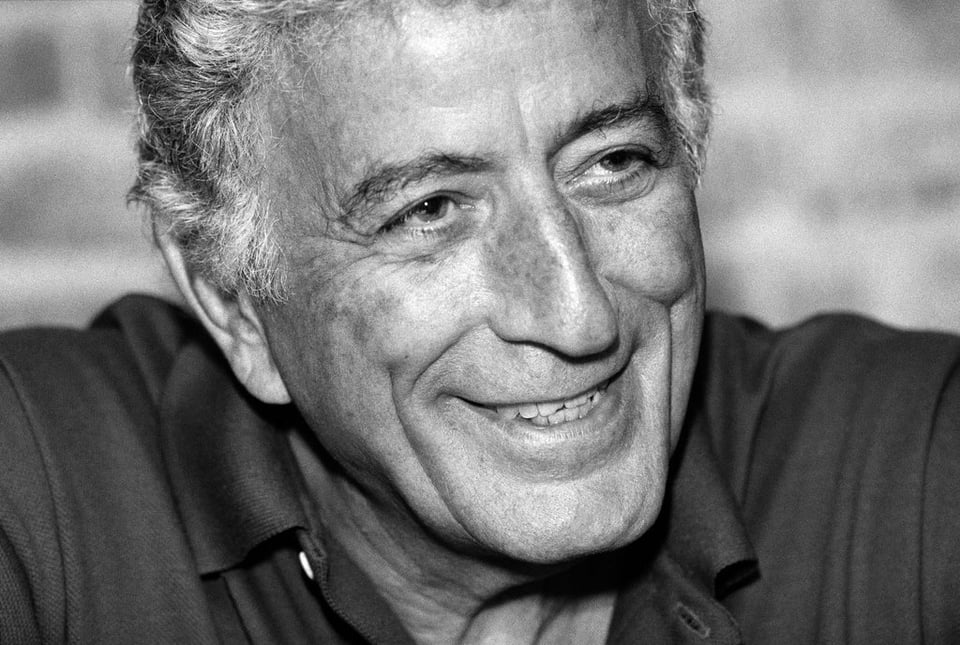
Tony Bennett. The Legend. 1927-2023.
 ________________________
________________________